Hospital Price Transparency: From Washington, D.C., to Austin, Texas, and Beyond
B A C K G R O U N D
The high cost of healthcare in the U.S. affects the health and financial well-being of Americans. In 2019, the U.S. spent 17.7 percent of its Gross Domestic Product on healthcare, equating to approximately $3.8 trillion in annual health expenditures (Martin et al., 2020). That same year, 33 percent of Americans surveyed reported to the Gallup Poll that they or a family member put off medical care because of the cost, with 25 percent delaying care for a serious condition (Saad, 2019). Policies that remove uncertainty about the cost of medical care enhance the ability for families to plan their finances around future healthcare expenses and make comparisons across providers, which may lead to fewer people delaying necessary care. This could result in better outcomes regarding disease prevention and treatment as well as overall health nationwide. Hospital price transparency, if successfully implemented, is one policy solution with the potential to demonstrate this impact while also putting pressure on providers to create greater value for patients.
On November 15, 2019, the Centers for Medicare and Medicaid Services (CMS) finalized a rule effective January 1, 2021, requiring hospitals operating in the United States to provide clear, accessible pricing information online by making it publicly available in two mechanisms: 1) a machine-readable file containing a list of five types of standard charges, including those negotiated with insurers, for all items and services, and 2) a consumer-friendly list of the same five types of standard charges for a limited set of shoppable services (HHS, 2019). For the second mechanism, the rule requires the display of 70 CMS-specified shoppable services that will be standard across all hospitals and another at least 230 hospital-selected shoppable services for a combined total of at least 300 shoppable services at each hospital.
Price transparency in healthcare is not a new idea, considering that it was the experiences of states, insurers, and self-funded employers finding evidence of the cost-reducing benefits of transparency that significantly influenced the promulgation of the CMS Hospital Price Transparency Rule (HHS, 2019). While many states had previously passed laws to establish price transparency websites or mandate price HOSPITAL PRICE TRANSPARENCY From Washington, D.C., to Austin, Texas, and Beyond By: Heidi Overton, M.D., and David Balat information be made available to consumers, there were significant gaps in the ability of Americans to access this information and evidence of low-uptake due to reported barriers by patients (Semigran et al., 2017). As of July 2019, a Pioneer Institute study found a lack of robust price transparency laws in states, with only six meeting their criteria for top-tier designation and 11 meeting second-tier criteria (DiBiase et al., 2020). The new federal rule intended to fill those gaps so that all Americans could reliably access hospital standard charge data and benefit from the primary goal of price transparency—empowerment through increased control over their healthcare costs.
This white paper explores the need for hospital price transparency, evaluates the variable implementation of the CMS Hospital Price Transparency Rule, examines current Texas legislation as one model of state-based price transparency solutions, and discusses future implications.
W H Y P R I C E T R A N S P A R E N C Y I S N E E D E D
The high cost of healthcare is consistently one of the top concerns of Americans in national surveys. A Morning Consult/Politico national survey from May 5, 2021, found that 88 percent of Americans want Congress to prioritize reducing healthcare costs, with 59 percent reporting this as their top priority (Morning Consult, 2021). While there is bipartisan consensus to bring down costs, Americans generally have different views on the best mechanism to accomplish this goal. Price transparency is a stark exception. A 2019 Harvard-Harris poll showed that 88 percent of Americans favored requiring healthcare providers to disclose pricing information (HHP, 2019). In 2020, the Foundation for Government Accountability also found that 87 percent of those polled supported healthcare price transparency as a way to help control costs and increase access for their families (FGA, 2020). Americans are resoundingly clear that they want to see lower healthcare costs, and they believe price transparency is a crucial tool to making that a reality.
Many studies, particularly over the past decade, have shown dramatic price variations for the same medical care from different healthcare providers in the same geographic area with no difference in quality (U.S. GAO, 2014). The 2014 Government Accountability Office report illustrated this with the following example:
“…the cost for maternity care at selected acute care hospitals in Boston, all of which rated highly on several quality indicators, ranged between $6,834 and $21,554 in July 2014” (U.S. GAO, 2014, p. 12).
Without the ability to know and accept prices beforehand, Americans are left to navigate the healthcare system blindfolded—particularly during the most pivotal moments of life. High and variable healthcare costs can also contribute to medical debt, which the Urban Institute has found currently affects 15 percent of Americans (Urban Institute, n.d.). Beyond this, studies have shown that wage garnishment for unpaid medical bills can be more prevalent at some hospitals, unbeknownst to patients at the time they seek care (Bruhn et al., 2019). The Consumer Financial Protection Bureau reports that approximately 20 percent of consumer credit reports have at least one medical debt collection tradeline, and more than half of all collection tradelines are due to unpaid medical bills (CFPB, 2014).
Hospital price transparency is about more than financial transactions—it is about the patient and consumer empowerment and establishing trust with their medical providers. It allows individuals to make informed choices about how and when to receive the medical care they need without feeling financially vulnerable at each appointment or procedure.
V A R I A B L E I M P L E M E N T A T I O N
Although the CMS Hospital Price Transparency Rule has been in effect for over 5 months now, there has been variable implementation by hospitals thus far according to several analyses, which are summarized below:
- An early analysis of the 20 largest hospitals in the country by ADVI found that all hospitals had posted some information but not all fully met the rule requirements (ADVI, n.d.).
- A March 2021 Health Affairs study found that 65 of the largest hospitals in the U.S. were noncompliant with the regulation, and the remainder of the hospitals varied in their levels of compliance (Henderson & Mouslim, 2021).
- A Peterson-KFF analysis of the two largest hospitals in each state and D.C. (102 hospitals total) found that a majority of hospitals posted gross charges in consumer tools and machine-readable files, fewer posted discounted rates, and a minority posted payer-specific negotiated rates (Kurani et al., 2021). \
- The Texas Public Policy Foundation and the Health Cost Labs created a statelevel Price Transparency Compliance Index, which found that in May 2021, only 48 percent of hospitals were compliant with the regulation and with ranges from 82 percent in Minnesota to 12 percent in Maine (TPPF, n.d.).
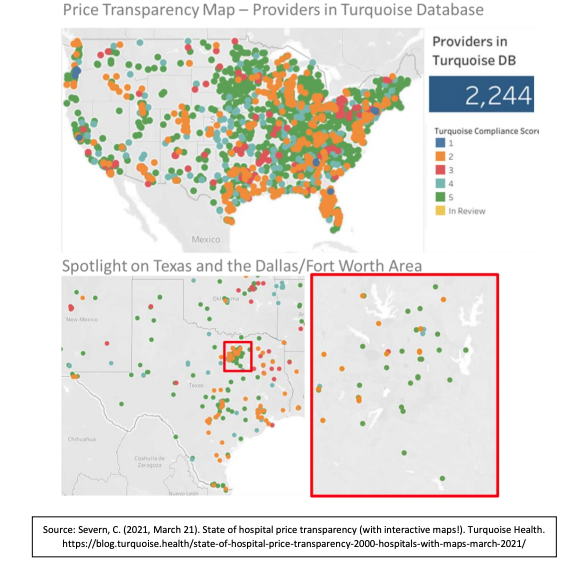
There are multiple reasons for this variable compliance, but a letter from the American Hospital Association (AHA) to former Secretary Azar on January 7, 2021, offers some insight into the concern of hospitals (AHA, 2021). The AHA requested enforcement discretion on the rule due to the following concerns: 1) limited hospital and health system resources to comply amid the COVID-19 public health emergency, 2) gaps in federal guidance, and 3) new statutory price transparency requirements. This request came after a federal appeals court ruled against an AHA legal challenge to the final rule (AHA v. Azar, 2020). Despite these requests from AHA, the rule remains in effect, and CMS recently sent out the first round of warning letters to non-compliant hospitals (Muoio, 2021). The start-up Turquoise Health has created a compliance score (1-5 stars with 5 stars being the highest/best compliance) and an interactive dashboard to facilitate research that moves the market towards transparency. Thus far, the Turquoise database has information for over 2200 of the approximately 6000 healthcare providers in the U.S. and provides hospital-level compliance information (Severn, 2021). The Turquoise interactive dashboard was utilized to explore the compliance variability described above, with spotlights on the state of Texas and the Dallas/Fort Worth Area.
Figure 1: Turquoise Health Database Price Transparency Compliance Map—U.S. and Texas
H O W P A T I E N T S C A N U S E P R I C E T R A N S P A R E N C Y T O O L S
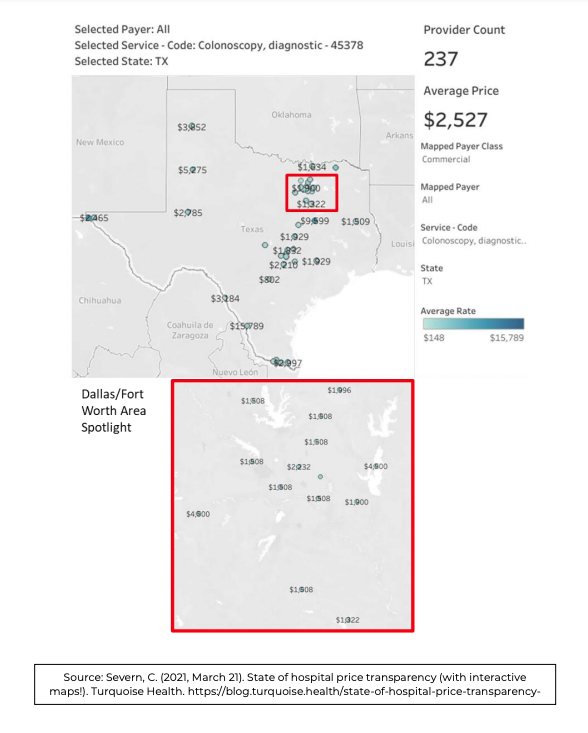
Americans have clearly supported price transparency, and now they can reap the benefits. For common, non-emergent procedures, consumers can evaluate prices at nearby hospitals and make an informed choice about where to receive care. Below is a demonstration using the Turquoise Health data of how individuals in the Dallas/Fort Worth area can benefit from having access to price transparency information. A diagnostic colonoscopy is a standard procedure that individuals generally undergo after a concerning finding during colorectal cancer screening. The price of this frequent procedure ranges from $148 to $15,789—a 100x multiplication.
Figure 2: Turquoise Health Database Price Transparency for Diagnostic Colonoscopies—Texas and Dallas/Fort Worth Area
T A K I N G C O N T R O L – T H E T E X A S E X A M P L E
CMS has already proposed repealing some of the requirements for transparency specifically targeted at Medicare Advantage insurers through the FY 2021 Hospital Inpatient Prospective Payment System Final Rule (CMS, 2021). This repeal and consequent weakening of transparency in one regulation may embolden opponents of transparency further to unravel requirements, such as those in the CMS Hospital Price Transparency Rule, that would contribute to building upon such valuable tools already mentioned. It is because of actions like these that we understand why the state legislatures are so incredibly important.
During the 87th Texas legislative session, Texas legislators have advanced a bill, S.B. 1137, that codifies the CMS Hospital Price Transparency Rule (Texas Legislature - 87(R) History for SB 1137, 2021). According to the Texas Senate Research Center bill analysis, the Sponsor’s statement of intent includes:
“The CMS rule is designed to increase market competition and lower healthcare costs by providing standard hospital pricing information to the public. State codification of the rule will ensure that price transparency and consumer empowerment will continue in Texas even if the rule is repealed or changed at the federal level. As proposed, S.B. 1137 amends current law relating to the required disclosure by hospitals of prices for hospital services and items, and provides administrative penalties” (Texas Senate Research Center, n.d.).
S.B. 1137 is an example of state policymakers putting the citizens of their state first by ensuring that transformative policy solutions are made permanent. Despite the variable implementation of the CMS Hospital Price Transparency Rule across the nation, Texas hospitals, if S.B. 1137 becomes law, will be required to comply, meaning Texans stand fully to reap the benefits of the policy. Other states should consider following this example to ensure maximal benefit for their citizens.
F U T U R E I M P L I C A T I O N S
Hospital price transparency is one tool to empower patients and lower healthcare costs to help improve the country’s health. Considering the inconsistent implementation of the CMS Hospital Price Transparency Rule across the U.S., the Texas example demonstrates the active role states can have in ensuring policies they believe will positively impact people in their state are made permanent.
The model of codifying federal regulatory policy at the state level is applicable beyond healthcare and should be considered in areas such as energy and the environment. It is a way to return power and control to the states to meet their citizens’ needs without being dependent on the federal bureaucracy. Importantly, it is a dynamic model of federalism that reinforces the goal of government at every level—to put its citizens first.
A U T H O R S B I O G R A P H I E S
Heidi Overton, M.D., is Director of the Center for a Healthy America at the America First Policy Institute.
David Balat is Director of the Right on Healthcare initiative at the Texas Public Policy Foundation.
W O R K S C I T E D
ADVI. (n.d.). Implementation of Newly Enacted Hospital Price Transparency. 2021. Retrieved May 17, 2021, from https://advi.com/analysis/Hospital_Transparency_- _ADVI_Summary.pdf
American Hospital Association. (2021, January 7). American Hospital Association Letter to HHS Secretary Azar on the Hospital Price Transparency Rule. https://www.aha.org/system/files/media/file/2021/01/aha-urges-hhs-exerciseenforcement-discretion-with-respect-hospital-price-transparency-rule-letter-1-7-20.pdf
American Hospital Association v. Azar, No. 20-5193 (D.C. Cir. 2020). Retrieved May 18, 2021, from https://www.cadc.uscourts.gov/internet/opinions.nsf/CCDF215AFCAF25F98525864D005716BC/$file/20-5193-1877500.pdf
Bruhn, W. E., Rutkow, L., Wang, P., Tinker, S. E., Fahim, C., Overton, H. N., & Makary, M. A. (2019). Prevalence and Characteristics of Virginia Hospitals Suing Patients and Garnishing Wages for Unpaid Medical Bills. In JAMA - Journal of the American Medical Association (Vol. 322, Issue 7, pp. 691–692). American Medical Association. https://doi.org/10.1001/jama.2019.9144
Centers for Medicare & Medicaid Services. (2021). Medicare Program; Hospital Inpatient Prospective Payment Systems for Acute Care Hospitals and the LongTerm Care Hospital Prospective Payment System and Proposed Policy Changes and Fiscal Year 2022 Rates; Quality Programs and Medicare Promoting Interoperability Program Requirements for Eligible Hospitals and Critical Access Hospitals; Proposed Changes to Medicaid Provider Enrollment; and Proposed Changes to the Medicare Shared Savings Program. Federal Register. https://www.federalregister.gov/documents/2021/05/10/2021-08888/medicareprogram-hospital-inpatient-prospective-payment-systems-for-acute-carehospitals-and-the
Consumer Financial Protection Bureau. (2014). Consumer credit reports: A study of medical and non-medical collections. https://files.consumerfinance.gov/f/201412_cfpb_reports_consumer-creditmedical-and-non-medical-collections.pdf
Department of Health and Human Services. (2019, November 27). Medicare and Medicaid Programs: CY 2020 Hospital Outpatient PPS Policy Changes and Payment Rates and Ambulatory Surgical Center Payment System Policy Changes and Payment Rates. Price Transparency Requirements for Hospitals To Make Standard Charges Public. Federal Register. https://www.federalregister.gov/documents/2019/11/27/2019-24931/medicareand-medicaid-programs-cy-2020-hospital-outpatient-pps-policy-changes-andpayment-rates-and
DiBiase, C., Corvese, L., Anthony, B., Archambault, J., & Chowdhury, S. (2020). Status of Healthcare Price Transparency across the United States. https://pioneerinstitute.org/transparency/national-study-finds-most-states-lackhealthcare-price-transparency-laws/ Foundation for Government Accountability. (2020, September 24). Voters Support Health Care Price Transparency. https://thefga.org/polling/voters-supporthealth-care-price-transparency/
Harvard - Harris Poll. (2019). https://harvardharrispoll.com/wpcontent/uploads/2019/06/HHP_May19_vF.pdf
Henderson, M., & Mouslim, M. C. (2021). Low Compliance From Big Hospitals On CMS’s Hospital Price Transparency Rule. https://www.healthaffairs.org/do/10.1377/hblog20210311.899634/full/
Himmelstein, D. U., Woolhandler, S., Lawless, R. M., Thorne, D., & Foohey, P. (2019). Medical bankruptcy: Still common despite the Affordable Care Act. In American Journal of Public Health (Vol. 109, Issue 3, pp. 431–433). American Public Health Association Inc. https://doi.org/10.2105/AJPH.2018.304901
Kurani, N., Ramirez, G., Hudman, J., Cynthia, C., & Kamal, R. (2021, April 9). Early results from federal price transparency rule show difficulty in estimating the cost of care. Peterson-KFF Health System Tracker. https://www.healthsystemtracker.org/brief/early-results-from-federal-pricetransparency-rule-show-difficultly-in-estimating-the-cost-ofcare/?mkt_tok=ODUwLVRBQS01MTEAAAF8aiDVWxbfgM4A_xGGEWDDaTd1LGomnG4MNh0I9Y4cSxsg1kL9BMI5KFodIneygYI oMsyLNTqAT7KOM47XRTZn
Martin, A. B., Hartman, M., Lassman, D., & Catlin, A. (2020). National health care spending in 2019: Steady growth for the fourth consecutive year. Health Affairs, 40(1), 14–24. https://doi.org/10.1377/hlthaff.2020.02022
Morning Consult. (2021, May 5). Top 2 Issues Are Health Care Costs & Drug Costs — Protect Our Care. https://www.protectourcare.org/new-morning-consult-polltop-2-issues-are-health-care-costs-drugcosts/?utm_source=rss&utm_medium=rss&utm_campaign=new-morningconsult-poll-top-2-issues-are-health-care-costs-drug-costs
Muoio, D. (2021, May 10). CMS sent out warnings to hospitals failing at price transparency. Some still aren’t sure where they land. FIERCE Healthcare. https://www.fiercehealthcare.com/hospitals/cms-sent-out-its-first-wavewarnings-to-hospitals-noncompliant-its-new-price-transparency
Saad, L. (2019). More Americans Delaying Medical Treatment Due to Cost. Gallup. https://news.gallup.com/poll/269138/americans-delaying-medical-treatmentdue-cost.aspx
Semigran, H. L., Gourevitch, R., Sinaiko, A. D., Cowling, D., & Mehrotra, A. (2017). Patients’ Views on Price Shopping and Price Transparency. The American Journal of Managed Care, 23(6). https://www.ajmc.com/view/patients-views-onprice-shopping-and-price-transparency
Severn, C. (2021, March 21). State of hospital price transparency (with interactive maps!). Turquoise Health. https://blog.turquoise.health/state-of-hospital-pricetransparency-2000-hospitals-with-maps-march-2021/
Texas Legislature - 87(R) History for SB 1137. (2021). https://capitol.texas.gov/BillLookup/History.aspx?LegSess=87R&Bill=SB1137
Texas Public Policy Foundation. (n.d.). The Price Transparency Compliance Index. Retrieved May 17, 2021, from https://www.texaspolicy.com/transparency/ Texas Senate Research Center. (n.d.). Bill Analysis - S.B. 1137. Retrieved May 18, 2021, from https://capitol.texas.gov/tlodocs/87R/analysis/html/SB01137I.htm
United States Government Accountability Office. (2014). HEALTH CARE TRANSPARENCY Actions Needed to Improve Cost and Quality Information for Consumers Report to Congressional Requesters United States Government Accountability Office. https://www.gao.gov/assets/gao-15-11.pdf
Urban Institute. (n.d.). Debt in America: An Interactive Map. 2021. Retrieved May 17, 2021, from https://apps.urban.org/features/debt-interactivemap/?type=medical&variable=perc_debt_med
